Our therapy team consists of Physiotherapy, Speech & Language, Dietetics & Pharmacy; we work closely with the nurses, health care assistants and doctors to care for our patients. Every day we discuss the medical needs and goals for each patient. We work closely to individualise our care and rehabilitation for each patient.
Rehabilitation is a journey and the therapy team will work alongside our patients from admission to the unit, through to step-down to the ward. Therapy will continue throughout the patients stay in hospital, until discharge.
Who’s who:
Abi Oliver- REHABILITATION COORDINATOR & ADVANCED PRACTICE PHYSIOTHERAPIST
ROLE:
- To lead and coordinate the ventilator weaning
- To lead the Therapy Team
- To coordinate the rehabilitation of patients in the Critical care unit.
PHYSIOTHERAPY TEAM
Abi Oliver, Kate Baker, Chris Gautrey and Anna Williams- Critical Care Physiotherapists
ROLE:
Physiotherapists assess patients on critical care, the listen to their lungs and assess their respiratory function. They clear sputum from patients’ lungs, teach breathing exercises and encourage them to cough. They also assist patients in getting out of bed and mobilising. Exercises are prescribed and goals are set to help patients return to their usual function and mobility.
The role of the ICU physiotherapist
PATIENT CENTRED CARE
We aim to involve our patients and their families when we set rehabilitation goals, it is important that we make goals specific and realistic for each individual. We like to make patients feel as comfortable as possible.
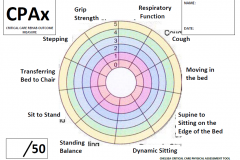
OUTCOME MEASURES
We use a nationally recognised Critical care Outcome measure to give a visual representation of our patients’ progress and rehabilitation needs- ‘CPAX Score’, this will be displayed on the patients rehabilitation board as below:
REHABILITATION EQUIPMENT
Early mobilisation is very important for patients on the Critical Care Unit. Many patients on the unit have lots of muscle weakness and need assistants to move and even roll over in bed. Patients who are on a ventilator (breathing machine) may need sedation (medication) and require expert handling and specialised equipment to facilitate their early rehabilitation. We know that early rehabilitation is likely to improve long term outcomes for the patient health and quality of life.
‘Rehabilitation after critical illness in adults’ NICE GUIDANCE CG083
To allow us to sit patients out of bed when they are unable to independently sit or stand we have a specialist chair- “The Combilizer” it allows us to slide a patient out of bed flat and can be positioned into sitting or a standing position with safety straps.
<<<MORE IMAGES HERE>>>
FUNDRAISING
We are always in need of more equipment for our patients and regularly fundraise, please see our fundraising page!
VENTILATOR WEANING
Weaning from a ventilator can be a slow process, if you have been on a ventilator (breathing machine) for some time your breathing muscles become weak and inactive. It is often necessary to perform a tracheostomy to allow the gradually reduction of ventilator support to allow breathing muscles to strengthen. This also means we can communicate, get out of bed and rehabilitate earlier.
The ‘weaning process’ is a team approach but it is led at Southport Critical Care by the Rehabilitation Coordinator. 24/7 weaning & rehabilitation plans are drawn up on the patients ‘Rehabilitation Board’. The plans map out the times for ventilator support pressures to be reduced and rehabilitation plans for the day. This joined up approach has proven very successful in getting our patients mobile and off support by the time they are ready to step-down the ward level care.
Goals are created in conjunction with the patient for example- trial of speaking valve, Zoom video calls with family, standing in tilt table and going outside.
<<<IMAGES HERE>>>